[ad_1]

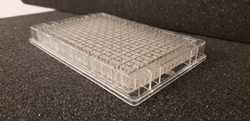
PREDICT96 is an organ-on-a-chip device seamlessly configured into an industry-standard multiwell cell culture plate.
As the global pandemic of COVID-19 continues to grow, our system has the potential to quickly evaluate antiviral and repurposed drugs to help combat this devastating disease. – Ashley Gard, Senior Member of the Technical Staff, Draper
CAMBRIDGE, Mass. (PRWEB)
June 23, 2020
Draper today announced the release of a new scientific article that describes how the company’s technology can be used to test an in vitro human lung model to investigate responses following infection with COVID-19 and influenza. The study was part of a collaboration between Draper and the University of Massachusetts Medical School. The manuscript, titled “High-Throughput Human Primary Cell-Based Airway Model for Evaluating Influenza, Coronavirus, or other Respiratory Viruses in vitro,” was posted in bioRxiv.
Several preclinical research tools are available to model respiratory infections, but due to the complexity of the human lung and requirements to accurately model host-virus interactions, these models provide a poor correlation as a basis for guiding clinical strategy. As many scientists are asking for models with stronger in vitro-in vivo correlation, the scientific community begins to turn more towards using organ-on-a-chip systems as a cost-effective and more accurate way to develop therapies.
Draper, in collaboration with UMass Medical School, describe an in vitro, microfluidic system containing functioning patient-derived human airway cells, which mature into human lung tissue that researchers monitored using integrated sensing and studied following controlled exposure to infectious respiratory pathogens. The PREDICT96 platform allows scientists to accurately mimic the structure and function of human lung tissues derived from donors with different patient profiles and sustain human tissue organ models for several weeks of automated testing.
“One of the greatest barriers to the development of effective therapeutic agents to treat influenza, coronaviruses and many other infections of the respiratory tract is the absence of a robust preclinical model. As the global pandemic of COVID-19 continues to grow, our system has the potential to quickly evaluate antiviral and repurposed drugs to help combat this devastating disease,” said Ashley Gard, Senior Member of the Technical Staff at Draper.
Current preclinical models typically rely on high-throughput, low-fidelity in vitro screening with cell lines or low-throughput animal models that often provide a poor correlation to human clinical responses. Emerging organ-on-chip models have the potential to overcome these limitations, but are often designed for research environments and are often incompatible with workflows and standard instrumentation in pharmaceutical laboratories.
In contrast, PREDICT96 is an organ-on-a-chip device seamlessly configured into an industry-standard multiwell cell culture plate, comprising 96 individual co-culture devices and a perfusion system driven by 192 microfluidic pumps integrated into the plate lid. Pairs of microchannels within each device, each less than a millimeter in diameter, are separated by a biomimetic semi-permeable membrane lined with human cells and arranged in complex configurations to support growth of human tissue. The device enables researchers to grow 96 human lung tissues at once and conduct 96 simultaneous experiments in order to evaluate different respiratory viruses, viral doses, viral strains and tissue from unique donors.
In the study, researchers evaluated the lung model’s responses to influenza A virus (IAV) and coronavirus (HCoV-NL63) and observed the behavior of airway cells in response to different therapeutic drug regimens. Results indicate that PREDICT96 can be used to model the human lung and its response to IAV and coronavirus infections, and could potentially be used to screen the efficacy of candidate therapeutics in a clinically relevant manner.
“The most striking features of our organ-on-a-chip is that it captures different reactions to respiratory viral infection by influenza and coronavirus, as well as detected expressions of ACE2 and TMPRSS2,” said Joe Charest, Ph.D., Head of Strategy and Business Development, Pharmaceutical R&D Technologies at Draper. The ACE2 receptor and TMPRSS2 protein play key roles in COVID-19 infections, and their presence is critical to the ability to model the infection process. Draper has expanded use of PREDICT96 beyond testing drug interactions with liver, kidney, vascular, gum and gastrointestinal tissue models to the new application for COVID-19, Charest added.
Funding was provided by Draper for the coronavirus research and by Defense Advanced Research Projects Agency (DARPA) for the influenza A virus research under its PREPARE program. Last year Draper and UMass Medical School, while working on the PREPARE program, announced the first instance of a dynamic air-liquid interface model using patient-derived cells for influenza testing.
Dr. Robert W. Finberg, an investigator on the team and chair of Medicine at UMass Medical School and UMass Memorial Medical Center, said COVID-19 is a natural extension of the PREPARE research. “Several of us working primarily on influenza are very excited about working on this new virus and finding different ways to prevent the disease it causes,” he said.
To read the full manuscript, please visit https://www.biorxiv.org/content/10.1101/2020.05.23.112797v1
Share article on social media or email:
[ad_2]