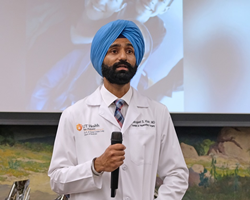
Tarunjeet Klair, M.D., of the Long School of Medicine at The University of Texas Health Science Center at San Antonio, treats University Transplant Center patients at University Hospital.
“For a healthy person to come and go through this for somebody else is not an easy thing.” – Tarunjeet Klair, M.D., assistant professor of surgery in the Long School of Medicine at The University of Texas Health Science Center at San Antonio and surgical director of the Living Liver Donor Program
SAN ANTONIO (PRWEB)
January 29, 2020
A major emphasis by the American Society of Transplant Surgeons is to increase organ donation in order to save the lives of patients suffering from end-stage organ failure. Currently an estimated 15% of patients die while on the waiting list in the United States because there are insufficient organs to meet this lifesaving demand. Decreasing the waiting list mortality requires more organs being procured from both deceased and living donors, which in turn requires innovation and organ preservation research. In San Antonio, Texas, transplant surgeons at the Long School of Medicine of The University of Texas Health Science Center at San Antonio innovated an effective approach to maximize the altruistic desire and contributions of living liver donors.
A conundrum last April
Anna Moreno hoped to donate part of her liver to save her father, Mark Blair. Natasha Sanchez felt led by God to give part of her liver to her friend, Sarah D’Angelo. Then the tests came in. Anna wasn’t a match for her father. Natasha, however, was a match for both D’Angelo and Blair.
What to do? Anna Moreno and Natasha Sanchez had both prepared to be living liver donors at University Transplant Center, a clinical partnership combining the excellence of physicians in the Long School of Medicine with the technology and support teams of University Health System.
Tarunjeet Klair, M.D., assistant professor of surgery in the Long School of Medicine and surgical director of the Living Liver Donor Program, suggested an alternative – swap donors so that both recipients could receive a transplant.
On two days in April 2019, the transplant team performed the transplants that saved Mark Blair and Sarah D’Angelo. Recovery progressed, and the following October, University Transplant Center welcomed the recipients and donors for a reunion of themselves and members of the transplant team.
The paired exchange was the first in the U.S. for living liver transplants, as far as the transplant center’s program directors are aware. The team performed a second paired exchange in July.
Living liver programs are rare
University Transplant Center is among only three dozen transplant centers nationwide – including three in Texas – that perform living liver transplants. In both 2018 and 2019, the transplant center was the second largest program in the United States in the number of living liver transplants.
Many centers do not have experience with living liver donors, and paired exchanges require specialized surgical training and expertise. “Given the large volume of very successful living donor transplant cases managed by our team, who also perform a large number of complex liver resections annually to remove cancers and other lesions in the liver, our center knew we had the safety record, standards and expert team members in place to save more patients through paired exchange,” Dr. Klair said.
Success in living donor liver transplantation requires four highly trained surgeons and a robust team of professionals including transplant hepatologists, nutritionists, nurses and social workers, to name a few. University Transplant Center comprises a cadre of professionals who follow the patients through their journeys from illness to recovery. Many team members, as faculty of the Long School of Medicine, are involved in transplant research and health professional education.
The recent success with living donors is built upon a strong foundation of deceased donor liver transplantation over three decades and a comprehensive and talented team. Glenn A. Halff, M.D., professor of surgery in the Long School of Medicine, inaugurated the liver transplant program in 1993, and within five years the transplant center was performing more than 100 liver transplants a year, far exceeding expectations.
Shortening the waiting list
Long School of Medicine pediatric and transplant surgeon Francisco G. Cigarroa, M.D., who directs University Transplant Center, joins Dr. Halff, Dr. Klair and the entire team in promoting living liver donation as a long-term solution for the shortage of deceased donors. A transplant center needs to develop a broad culture of advocating for living donation and associated comprehensive education for interested living donors. Late last year, almost 13,000 people were on the national liver transplant wait list, including nearly 1,400 in Texas.
“We strive to shorten the waiting list to transplantation through multiple innovative approaches including living donor liver transplants,” Dr. Cigarroa said.
The liver is the largest organ in the body. Among its many functions, it secretes bile, which aids digestion. Because the liver possesses the amazing ability to regrow, surgeons may remove a portion of the liver of a healthy individual to transplant into a person whose liver is diseased. Within a couple of months, the donor’s remaining liver regrows to a normal size, while the portion of liver transplanted into the recipient also grows and restores healthy liver function.
This is a lifesaver for recipients who need a liver transplant due to cancer, cirrhosis (scarring) or other disease. They can avoid having to become very sick while waiting for a matching liver from a deceased donor. It is a wait that unfortunately some patients don’t survive.
Surgeon’s vision
The innovation of paired exchanges ensures compatibility of living liver donations between well-prepared donors and waiting recipients. Dr. Klair’s inspiration made it happen.
“Dr. Klair has an unrelenting commitment to the safety and well-being of our patients, and where donor supply falls short, he is always looking for a solution to bridge the gap and make sure that we can give a safe alternative to our patients,” said Jennifer Milton, RN, chief administrative officer of University Transplant Center.
Accordingly, the center increased living liver transplants from six in 2017 to 39 in 2019.
The living liver paired exchange also requires patients and families to trust their medical providers. “For a healthy person – who doesn’t need an operation – to come and go through this for somebody else is not an easy thing,” Dr. Klair said. “We recognize that.”
Mark Blair and Sarah D’Angelo, with a new lease on life thanks to their “liver buddies” Natasha Sanchez and Anna Moreno, are among the grateful beneficiaries.
The Long School of Medicine at The University of Texas Health Science Center at San Antonio is named for Texas philanthropists Joe R. and Teresa Lozano Long. The school is the largest educator of physicians in South Texas, many of whom remain in San Antonio and the region to practice medicine. The school teaches more than 900 students and trains 800 residents each year. As a beacon of multicultural sensitivity, the school annually exceeds the national medical school average of Hispanic students enrolled. The school’s clinical practice is the largest multidisciplinary medical group in South Texas with 850 physicians in more than 100 specialties. The school has a highly productive research enterprise where world leaders in Alzheimer’s disease, diabetes, cancer, aging, heart disease, kidney disease and many other fields are translating molecular discoveries into new therapies. The Long School of Medicine is home to a National Cancer Institute-designated cancer center known for prolific clinical trials and drug development programs, as well as a world-renowned center for aging and related diseases.
The University of Texas Health Science Center at San Antonio, dba UT Health San Antonio, is one of the country’s leading health sciences universities and is designated as a Hispanic-Serving Institution by the U.S. Department of Education. With missions of teaching, research, healing and community engagement, its schools of medicine, nursing, dentistry, health professions and graduate biomedical sciences have graduated more than 37,000 alumni who are leading change, advancing their fields, and renewing hope for patients and their families throughout South Texas and the world. To learn about the many ways “We make lives better®,” visit http://www.uthscsa.edu.
Stay connected with The University of Texas Health Science Center at San Antonio on Facebook, Twitter, LinkedIn, Instagram and YouTube.