Clotting in really sick COVID-19 patients is not something trivial and unimportant — it may well be fundamental to what is going on.
LOMA LINDA, Calif. (PRWEB)
August 25, 2021
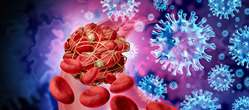
Loma Linda University Health researchers say severely ill COVID-19 patients likely die as the result of micro clots formed in the lungs that spread to cause deadly damage to organs throughout the body. This finding from a recent study is different from the current understanding that the COVID-19 virus travels to the body’s organs and damages blood vessel lining in those organs.
Once the clotting process begins, the body is no longer fighting against the virus but mostly against the clotting process instead, the study’s researchers said.
The findings, which may advance an understanding of the disease that has claimed four million lives and counting, also call for a shift in the nature of the search for effective therapeutic solutions.
“This could change our approach to fighting this disease because we may have been looking in the wrong place,” says Brian Bull, MD, a pathologist, former dean of the Loma Linda University School of Medicine, and the study’s first author. “We have been looking for a treatment against a viral disease, but we should now also look for therapy for a viral disease that has transformed into a clotting disorder.”
The study, “A macrophage attack culminating in microthromboses characterizes COVID 19 pneumonia,” published in the Journal of Immunity, Inflammation and Disease, proposes an explanation for why COVID-19 patients die from a vast array of conditions such as strokes, heart attacks, kidney failure, or failure of several organs at the same time.
“We face the problem of not yet understanding the physiological disorders well enough to explain how a viral disease like COVID-19 kills people in such a diverse and difficult-to-predict fashion.” Bull says.
Bull and co-author Karen Hay contend that showers of tiny clots form and block micro-blood vessels in the bodies of many severely ill COVID-19 patients. Though invisible to the naked eye, the micro clots can damage and kill tiny portions of whichever organ tissue — brain, heart, liver, kidney, lung, etc. — the blocked blood vessels feed.
But how do these micro clots form and travel throughout the body? Bull provides a broad overview of this disease process:
-
When the body senses a COVID-19 infection, large white blood cells called monocytes respond and gather in the air sacs of the lungs. - Over the course of a few days, the monocytes transform into macrophages — the “demolition and cleanout crew” for infected and damaged tissue in the body. The macrophages attack the virus-laden cells that line the inside of the air sacs . Unfortunately, macrophages may also chew right through the virus-laden air sac lining to the blood vessels that surround each air sac. This is the place in the body where the blood picks up oxygen when we breathe. If the macrophages puncture these blood vessels the air sac will fill up with blood.
- A protein produced by the macrophages on their surfaces causes the blood to clot.
- When a clot forms an enzyme, thrombin, interacts with a protein in the blood known as fibrinogen to produce fibrin strands or fibrils. When these fibrin strands accumulate, they become a clot. These fibrils can be still soluble if they remain short enough (about 25 molecules or less). Anything longer than that becomes insoluble and will appear as tiny clots.
- Short chains of fibrin, still soluble, can travel in the blood supply to all of the body’s organs. As long as the fibrin chains remain short, this will cause no problems, but if more thrombin is coming from clots in the lungs, then more fibrin is continually being fed into the blood. This makes the chains of fibrin grow longer; they grow too long to remain in solution and showers of microclots will form.
- These micro clots will block the tiny blood vessels that nourish the tissue making up each of the body’s organs, making the organs less able to perform their necessary function. The organs (heart, kidney, brain, etc.) with little patches of dead and dying tissue throughout will, sooner or later, fail.
Indeed, when Bull and Hay monitored three COVID-19 patients hospitalized in an intensive care unit for tell-tale clotting biomarkers — the still soluble fibrin chains — they found that in a matter of four days, all of the fibrinogen in the patients’ bodies had transformed into soluble fibrin chains at levels five times higher than normal. Body organs were severely damaged in all three patients. Two of them died in the hospital, and the third survived but suffered severe brain damage.
Although Bull and Hay found blood clotting was taking place by tracking the bio-markers and performing clotting tests, no visible clots were detected in any of the three patients. The likeliest explanation, Bull states, is that those clots were present but were too small to be seen.
“Here in this study we have three patients in which clearly a massive clotting disorder occurred over a very short period,” Bull says.
Bull said in a year and a half of searching for therapeutic modalities, the medical community has not come up with any anti-viral medications that have had a significant beneficial effect on COVID-19. Yet, heparin, an anti-clotting drug, not an anti-viral medication, has proven highly beneficial and is now being given to virtually all hospitalized, severely ill COVID-19 patients.
“Clotting in really sick COVID-19 patients is not something trivial and unimportant — it may well be fundamental to what is going on,” Bull says.
To learn more about research at LLU, visit researchaffairs.llu.edu or call 909-558-8544.
Share article on social media or email: