A digital marker for coronary artery disease derived from machine learning and electronic health records can better quantify where an individual falls on the disease spectrum.
NEW YORK (PRWEB)
December 21, 2022
Using machine learning and clinical data from electronic health records, researchers at the Icahn School of Medicine at Mount Sinai in New York constructed an in silico, or computer-derived, marker for coronary artery disease (CAD) to better measure clinically important characterizations of the disease.
The findings, published online on December 20 in The Lancet, may lead to more targeted diagnosis and better disease management of CAD, the most common type of heart disease and a leading cause of death worldwide. The study is the first known research to map characteristics of CAD on a spectrum. Previous studies have focused only on whether or not a patient has CAD.
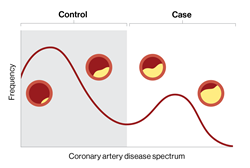
CAD and other common conditions exist on a spectrum of disease; each individual’s mix of risk factors and disease processes determines where they fall on the spectrum. However, most such studies break this disease spectrum into rigid classes of case (patient has disease) or control (patient does not have disease). This may result in missed diagnoses, inappropriate management, and poorer clinical outcomes, say the investigators.
“The information gained from this non-invasive staging of disease could empower clinicians by more accurately assessing patient status and, therefore, inform the development of more targeted treatment plans,” says Ron Do, PhD, senior study author and the Charles Bronfman Professor in Personalized Medicine at the Icahn School of Medicine at Mount Sinai. “Our model delineates coronary artery disease patient populations on a disease spectrum; this could provide more insights into disease progression and how those affected will respond to treatment. Having the ability to reveal distinct gradations of disease risk, atherosclerosis, and survival, for example, which may otherwise be missed with a conventional binary framework, is critical.”
In the retrospective study, the researchers trained the machine learning model, named in silico score for coronary artery disease or ISCAD, to accurately measure CAD on a spectrum using more than 80,000 electronic health records from two large health system-based biobanks, the BioMe Biobank at the Mount Sinai Health System and the UK Biobank.
The model, which the researchers termed a “digital marker,” incorporated hundreds of different clinical features from the electronic health record, including vital signs, laboratory test results, medications, symptoms, and diagnoses, and compared it to both an existing clinical score for CAD, which uses only a small number of predetermined features, and a genetic score for CAD.
The 95,935 participants included participants of African, Hispanic/Latino, Asian, and European ethnicities, as well as a large share of women. Most clinical and machine learning studies on CAD have focused on white European ethnicity.
The investigators found that the probabilities from the model accurately tracked the degree of narrowing of coronary arteries (coronary stenosis), mortality, and complications such as heart attack.
“Machine learning models like this could also benefit the health care industry at large by designing clinical trials based on appropriate patient stratification. It may also lead to more efficient data-driven individualized therapeutic strategies,” says lead author Iain S. Forrest, PhD, a postdoctoral fellow in the lab of Dr. Do and an MD/PhD student in the Medical Scientist Training Program at Icahn Mount Sinai. “Despite this progress, it is important to remember that physician and procedure-based diagnosis and management of coronary artery disease are not replaced by artificial intelligence, but rather potentially supported by ISCAD as another powerful tool in the clinician’s toolbox.”
Next, the investigators envision conducting a prospective large-scale study to further validate the clinical utility and actionability of ISCAD, including in other populations. They also plan to assess a more portable version of the model that can be used universally across health systems.
The paper is titled “Machine learning-based marker for coronary artery disease: derivation and validation in two longitudinal cohorts.” Additional co-authors are Ben O. Petrazzini, BS, Áine Duffy, MS, Joshua K. Park, BS, Carla Marquez-Luna, PhD, Daniel M. Jordan, PhD, Ghislain Rocheleau, PhD, Judy H. Cho, MD, Robert S. Rosenson, MD, and Jagat Narula MD, and Girish N. Nadkarni, MD.
The work was supported by funds from the National Institute of General Medical Sciences of the National Institutes of Health (NIH) grants T32-GM007280 and R35-GM124836, and by the National Heart, Lung, and Blood Institute of the NIH grants R01-HL139865 and R01-HL155915.
-####-
About the Icahn School of Medicine at Mount Sinai
The Icahn School of Medicine at Mount Sinai is internationally renowned for its outstanding research, educational, and clinical care programs. It is the sole academic partner for the eight-member hospitals* of the Mount Sinai Health System, one of the largest academic health systems in the United States, providing care to a large and diverse patient population.
Ranked 14th nationwide in National Institutes of Health (NIH) funding and among the 99th percentile in research dollars per investigator according to the Association of American Medical Colleges, Icahn Mount Sinai has a talented, productive, and successful faculty. More than 3,000 full-time scientists, educators, and clinicians work within and across 34 academic departments and 35 multidisciplinary institutes, a structure that facilitates tremendous collaboration and synergy. Our emphasis on translational research and therapeutics is evident in such diverse areas as genomics/big data, virology, neuroscience, cardiology, geriatrics, as well as gastrointestinal and liver diseases.
Icahn Mount Sinai offers highly competitive MD, PhD, and Master’s degree programs, with current enrollment of approximately 1,300 students. It has the largest graduate medical education program in the country, with more than 2,000 clinical residents and fellows training throughout the Health System. In addition, more than 550 postdoctoral research fellows are in training within the Health System.
A culture of innovation and discovery permeates every Icahn Mount Sinai program. Mount Sinai’s technology transfer office, one of the largest in the country, partners with faculty and trainees to pursue optimal commercialization of intellectual property to ensure that Mount Sinai discoveries and innovations translate into healthcare products and services that benefit the public.
Icahn Mount Sinai’s commitment to breakthrough science and clinical care is enhanced by academic affiliations that supplement and complement the School’s programs.
Through the Mount Sinai Innovation Partners (MSIP), the Health System facilitates the real-world application and commercialization of medical breakthroughs made at Mount Sinai. Additionally, MSIP develops research partnerships with industry leaders such as Merck & Co., AstraZeneca, Novo Nordisk, and others.
The Icahn School of Medicine at Mount Sinai is located in New York City on the border between the Upper East Side and East Harlem, and classroom teaching takes place on a campus facing Central Park. Icahn Mount Sinai’s location offers many opportunities to interact with and care for diverse communities. Learning extends well beyond the borders of our physical campus to the eight hospitals of the Mount Sinai Health System, our academic affiliates, and globally.
——————————————————-
*Mount Sinai Health System member hospitals: The Mount Sinai Hospital; Mount Sinai Beth Israel; Mount Sinai Brooklyn; Mount Sinai Morningside; Mount Sinai Queens; Mount Sinai South Nassau; Mount Sinai West; and New York Eye and Ear Infirmary of Mount Sinai.