“Being able to stop symptoms from progressing might mean that a patient could continue to drive to the store, to church or to another family member’s home. That ability is quickly lost if symptoms advance.” — Gabriel de Erausquin, MD, PhD, neurologist
SAN ANTONIO (PRWEB)
February 03, 2022
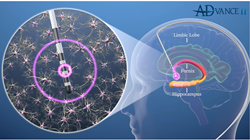
The University of Texas Health Science Center at San Antonio (UT Health San Antonio) and clinical partner University Health are among 27 sites worldwide (18 in the U.S., one in Canada and eight in Germany) evaluating the effectiveness of a technique called deep brain stimulation (DBS) in treating patients with mild Alzheimer’s disease. DBS is an established, nonpharmaceutical treatment that researchers hope could slow or even halt the progress of this devastating disease.
A San Antonio woman in her 70s underwent South Texas’ first DBS surgery for Alzheimer’s — one of the first 300 surgeries of its kind in the world — at University Hospital on Nov. 5, 2021. Alexander Papanastassiou, MD, associate professor of neurosurgery at UT Health San Antonio who sees University Health patients, implanted DBS electrodes during the operation. The surgery is minimally invasive to enhance rapid recovery with the least pain, blood loss and hospital time.
Gabriel de Erausquin, MD, PhD, professor of neurology at UT Health San Antonio and researcher with the health science center’s Glenn Biggs Institute for Alzheimer’s and Neurodegenerative Diseases, confirmed the electrode location by testing the patient’s heart rate and blood pressure responses to stimulation while she was awake during the procedure. The test stimulation also evoked a memory as it sometimes does. The patient went home the next day and returned Nov. 18 for the planned second stage of surgery to implant the generator in the chest wall. She went home the same day, recovered well, and returned Dec. 3 for randomization and initial programming.
A state-of-the-art robotic system, the Renishaw neuromate® purchased by University Health in 2017, aided the surgery. The robot has ensured accurate placement of brain implants to diagnose and treat epilepsy and movement disorders. Dr. Papanastassiou has performed scores of stereotactic robotic surgeries at University Health for those conditions. The neuromate® robot was invented by Peter Fox, MD, professor of radiology, neurology, psychiatry and physiology in the Joe R. and Teresa Lozano Long School of Medicine, UT Health San Antonio. He is director of the health science center’s Research Imaging Institute and has studied stereotactic technology to ensure precise targeting of transcranial magnetic stimulation for depression.
Stopping the decline
Evaluating DBS in Alzheimer’s disease is a new frontier. Dr. de Erausquin is the principal investigator and collaborating neurologist for the San Antonio site of the clinical trial. He has expertise in diagnosing and treating Alzheimer’s disease and movement disorders such as Parkinson’s disease, including experience gained from more than 200 DBS cases for movement disorders.
“The usual course of illness for people with early Alzheimer’s disease is a progressive loss of function that is very steady and doesn’t slow down,” Dr. de Erausquin said. “The purpose of this current trial is to test whether the device can help individuals with early Alzheimer’s disease to maintain their memory and independence.”
The study doesn’t aim to reverse disease progression. No current therapy does that. At this point, being able to arrest the decline in individuals who have a diagnosed form of Alzheimer’s and have symptoms would be a “major achievement,” Dr. de Erausquin said.
Precision
During stereotactic surgery, the surgical team secures a rigid frame to the skull. This establishes a 3D space for precise, computerized targeting of therapy delivery. The surgeon controls a robot to implant DBS electrodes in exact locations in the brain. Entry is gained through two dime-sized holes. Depending on the patient’s hairline, the only external mark may be a little bump on the skin.
“The electrodes are placed near a brain structure called the fornix, which is part of a circuit involved in the formation of memories,” Dr. Papanastassiou said. “The electrodes run underneath the skin down to a generator in the chest wall that is outside the ribcage and beneath the skin.”
Fine-tuning the effect
External instruments communicate with the generator. “Experienced programmers such as Dr. de Erausquin can change the amount of electrical current, the frequency, the pulse width and which of the electrodes are used to do the stimulation,” Dr. Papanastassiou said. “Different parameters are set based on how the patient is assigned in the study protocol.”
Because this is a clinical trial, some participants will be randomized to get stimulation earlier, with their generator being activated to deliver DBS soon after the implant. For other participants, the activation will be delayed by 12 months.
Programming sessions will look and feel the same to all patients, but some will be sham sessions that appear to initiate activation but do not. It is important that patients and physicians not be informed when a patient is receiving stimulation. This is to gain a true, unbiased measure of the procedure’s effectiveness in treating Alzheimer’s, Dr. de Erausquin said.
All patients in the study will receive the standard forms of treatment for early Alzheimer’s, no matter when their DBS is activated, he noted.
Jane’s story
The first San Antonio patient, named Jane, asked that her last name not be used. Turning 72 this spring, Jane was a 30-year teacher and librarian in a San Antonio school district before retiring in 2016. With degrees in English, nursing and library sciences, she also taught history but most enjoyed teaching health sciences to young people and taking them on rotations to a local hospital.
After leaving the classroom and library, life slowed down and she noticed little things about her memory.
“When I retired, I was by myself,” Jane said. “My husband was working, I didn’t know anyone, my friends were still working, and I was socially isolated for a while. I don’t know if that was what started it or not.”
Jane and her husband went to the Glenn Biggs Institute, where she was diagnosed. Dr. de Erausquin is one of her treating physicians and suggested she might join the DBS clinical trial.
Today the couple is active in a senior citizens’ group and Jane retains her interest in educating others. She soon will present a lecture titled “Jackie Robinson: Civil Rights Leader” to the group, in addition to showing a Robinson documentary and the film “42.”
“With Alzheimer’s disease, people automatically think a person is stupid and can’t do anything. That’s not the way it is,” Jane said. “I don’t want to be saddled with that burden.”
The Jackie Robinson lecture is an example, she said, of “things I’m really interested in, things I’m gung ho about, and I think it’s really neat.”
Saving daily living, for Jane and others
UT Health San Antonio and University Health are approved to do DBS implants in 12 patients with early Alzheimer’s disease.
“We are only enrolling people with early disease,” Dr. de Erausquin said. “DBS is most likely to be helpful early in the course of the illness. We seek people who already have symptoms and in whom it is confirmed, through analysis of proteins in the brain and spinal fluid, that Alzheimer’s disease is the underlying cause for those symptoms.
“Being able to stop symptoms from progressing might mean that a patient could continue to drive to the store, to church or to another family member’s home. That ability is quickly lost if symptoms advance,” Dr. de Erausquin said.
“I would give them a name and number of someone to contact,” Jane said, when asked what she would tell others who are interested to join the clinical trial. She said she had no pain after the DBS implantation.
For information on the clinical trial, including potential eligibility, visit http://www.MildAlzheimersStudy.com to see if you or your loved one may qualify for the study.
The University of Texas Health Science Center at San Antonio, also referred to as UT Health San Antonio, is one of the country’s leading health sciences universities and is designated as a Hispanic-Serving Institution by the U.S. Department of Education. With missions of teaching, research, patient care and community engagement, its schools of medicine, nursing, dentistry, health professions and graduate biomedical sciences have graduated 39,700 alumni who are leading change, advancing their fields, and renewing hope for patients and their families throughout South Texas and the world. To learn about the many ways “We make lives better®,” visit http://www.uthscsa.edu.
Stay connected with UT Health San Antonio on Facebook, Twitter, LinkedIn, Instagram and YouTube.
About University Health
University Health is San Antonio’s only locally owned health system and the only academic medical center in South Texas. Its University Hospital serves as the region’s Level I trauma center for adults and children, and is the only area hospital to be state-designated at the highest level for both its Maternity Center and Neonatal Intensive Care Unit. Outpatient care is provided through a comprehensive network of urgent, primary and specialty care centers. For more than 100 years, University Health has been committed to delivering compassionate, culturally competent and high-quality health care, based on a strong foundation of outcomes‐based research and innovative teaching. Learn more at UniversityHealthSystem.com. Follow us on Twitter and Facebook.